We don’t always tick like clocks and sometimes things can go wrong with us gynaecologically in a number of ways. Sometimes they are obvious and sometimes they are more hidden.
Here are just a few things which can go awry with your downstairs mix up.
And please remember….we’re all human and sometimes we do just get bad period pain. But if you suspect anything horrible, keep a diary, keep tracking and charting and go see your doctor.
Bad Period Pain
We all get this. Sometimes the witch comes with a vengeance. But what is normal and what’s not?
Well, pain mid cycle isn’t normal. Some women do have some pain when they ovulate but this shouldn’t be heavy cramping. It can be a sign of something not quite right if you’re having period like cramps outside your usual window for menstruating.
I personally think if you can’t control your period pains with over the counter medication like paracetamol or ibuprofen, or if you’re having to take them like sweets to keep going for more than a day or two, something isn’t right.
If you’re worried you may have something causing bad period pain then keep a diary of symptoms using this handy NHS diary or keep your App updated and then ask your GP. Do some research (we have a few of the common issues below) and push to see a gynaecologist. You should not have to suffer this. It isn’t a ‘curse anymore.
Heavy Bleeding or Light bleeding
What is the perfect period? The NHS have this handy tool (Are your periods heavy?) so please do have a go on this.
Short answer is:
The average amount of blood lost during a period is 30-40 millilitres (ml), with 9 out of 10 women losing less than 80ml. Heavy menstrual bleeding is considered to be 60ml or more in each cycle.
So if you are bleeding through a super tampon every hour for more than a day…you have got one heavy period. And it’s miserable. If you’re bleeding heavily and it’s impacting your day to day life, please go and see your GP. There are so many things they can do to help and they can investigate to see if anything else (see below) is causing it.
PCOS (Polycycstic Ovarian Syndrome)
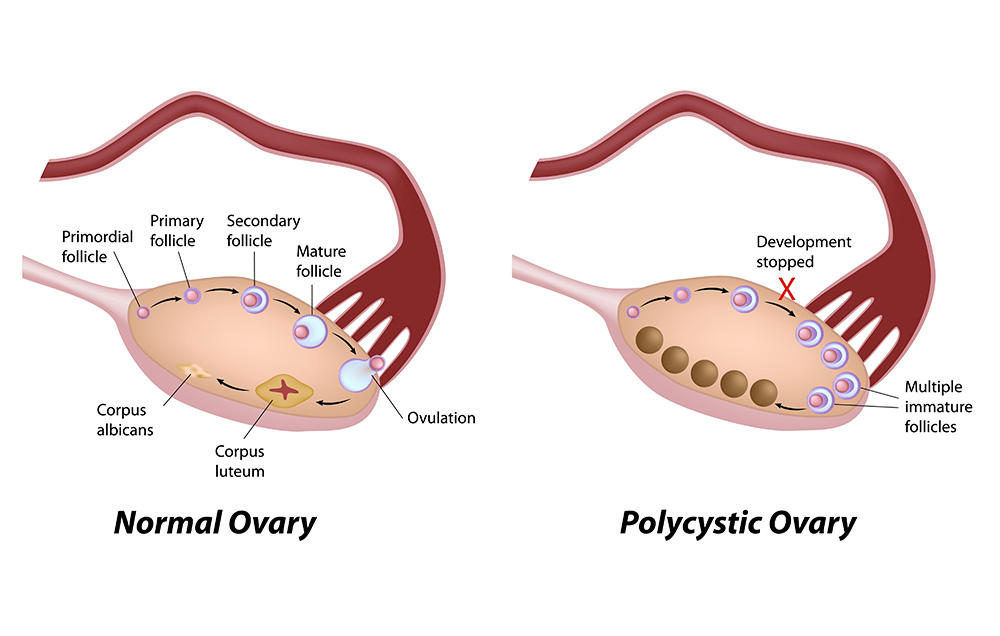
Polycystic Ovarian Syndrome is common and affects roughly 20% of women in the UK alone.
The term describes ovaries that contain many small teeny cysts usually no bigger than 8 millimeters each, located just below the surface of the ovaries. These cysts are egg-containing follicles that have not developed properly due to a number of hormonal abnormalities.
When women have the condition it comes with a few other symptoms on top of this.
These include:
- irregular periods, or a complete lack of periods
- irregular ovulation, or no ovulation at all
- reduced fertility – difficulty becoming pregnant
- unwanted facial or body hair (hirsutism)
- oily skin, acne
- thinning hair or hair loss from the scalp (alopecia)
- weight problems – being overweight, rapid weight gain, difficulty losing weight
- depression and mood changes
Some women will have all of these and others only some. An abnormal testosterone level often contributes to the symptoms. Long term it can lead to type 2 diabetes due to high insulin levels.
PCOS is usually diagnosed using a combination of an ultrasound scan to check for polycystic ovaries and blood tests to detect hormonal imbalances.
Your doctor should also check your blood pressure level and your blood sugar level. Once a diagnosis has been made, your doctor may refer you to a gynaecologist or an endocrinologist. You should also have annual monitoring of blood pressure and blood glucose levels.
The bad news is you can’t cure it. The good news is you can control it with a good, healthy diet and losing weight. It’s a bit boring but it significantly improves syndromes- just losing 5% of body weight in fact. Your health care provider can also sometimes help you find a contraceptive pill which can level out hormones and help control symptoms for the time being – it’s worth scheduling a chat with them.
Verity have some wonderful information on PCOS. If you think you have it please, get yourself to the GP and get it diagnosed now. This information is so useful to have and it will enable to you to start making changes to improving your long term reproductive health.
TTC with PCOS
If you decide you want to have children yes, it’s possibly going to be harder to conceive. But if you have diagnosed this issue and are prepared to use your plethora of knowledge to your advantage it is not a game changer. If you know you have PCOS and it has been properly diagnosed then I advise you to do the following:
- Once you have given yourself a month or two off contraception, chart for 3 months while having regular unprotected sex. If you have NOT ovulated chart for 3 months and aren’t pregnant in this time (e.g you can find no pattern of ovulation on your charts), don’t muck around. Get thyself to the GPs and insist on having your 7 day and 21 bloods done using your charts as evidence that you don’t think you’re ovulating. Go over your bloods with your doctor and push for a referral to a fertility clinic. There is no use fannying around for 6 months to a year if you’re not ovulating.
- Look into support drugs like clomid and femara which will help you to ovulate.
- Ask for an ultra sound to check that you do not have large cysts or tubal blockages.
Ovarian Cysts

Cysts can be painful and they should not be ignored!
“An ovarian cyst is a fluid-filled sac that develops on a woman’s ovary” (NHS)
Symptoms can include:
- pelvic pain – this can range from a dull, heavy sensation to a sudden, severe and sharp pain
- pain during sex
- difficulty emptying your bowels
- a frequent need to urinate
- heavy periods, irregular periods or lighter periods than normal
- bloating and a swollen tummy
- feeling very full after only eating a little
- difficulty getting pregnant – although fertility is unaffected in most women with ovarian cysts (see ovarian cysts and fertility)
If you have any of these get thee to thy doctor!
If your GP thinks you have a cyst they will book you in for an ultrasound. This will be monitored and if it looks like it is growing you will be referred to a gynaecologist. Personally, I’d push for a referral anyway if it’s causing significant pain.
They will also most likely push for blood tests to check that it is not cancerous.
In most cases the cyst will disappear on its own. In rarer cases they may need to operate to remove it
Fibroids
Growths that grow in your uterus, these are made of muscle and fibrous tissue Often symptom-less, some of the warning signs can be:
- heavy periods or painful periods
- tummy (abdominal) pain
- lower back pain
- a frequent need to urinate
- constipation
- pain or discomfort during sex
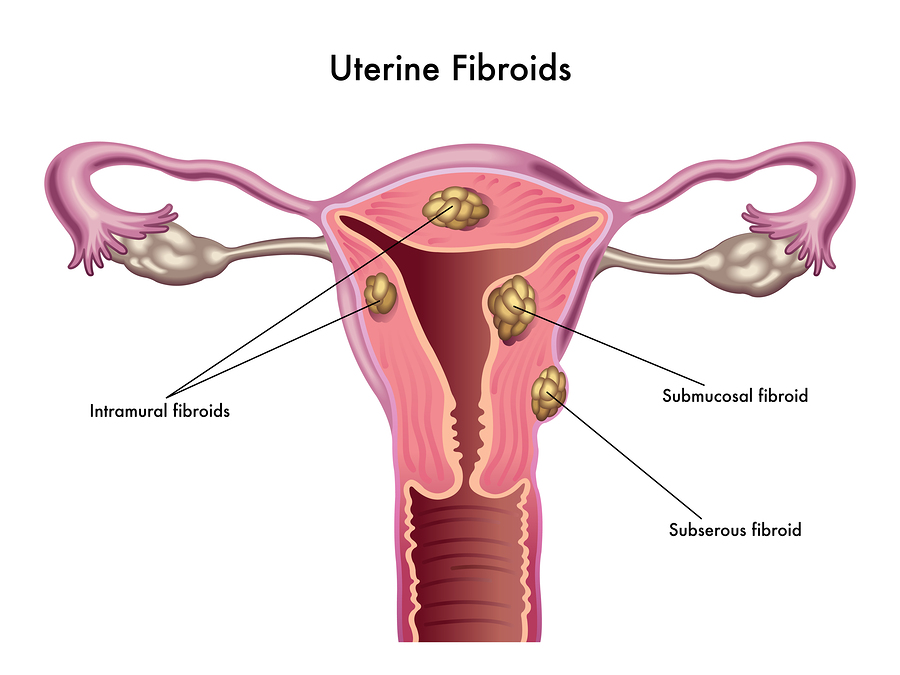
Linked to estrogen they are again one of life’s many crap mysteries. 1 in 3 of us women will have them with them occurring mostly between the ages of 30-50. They usually disappear with the menopause.
From the size of a pea to the size of a melon, you can have one or more of these nasties at a time. There are three types:
- intramural fibroids – the most common type which will develop in the muscle wall of the womb
- subserosal fibroids – fibroids that develop outside the wall of the womb into the pelvis and can become very large
- submucosal fibroids – fibroids that develop in the muscle layer beneath the womb’s inner lining and grow into the cavity of the womb
For more information see the NHS website and also their page on treatment.
Good news is, unless they’re causing pain or discomfort many will go away on their own. If they are causing irritation or pain please get to your GP who will send you to a gynaecologist to be scanned and investigated. They can cause issues when trying to conceive so again, it’s worth investigating before you try for children so you’re aware of any issues.
Polyps

These are non cancerous growths also found in the uterus. These little out growths in the womb can be around 1cm long and will often grow flattened to the lining. Very rarely they can develop into being cancerous.
Often there are no symptoms, but some can be among the following:
-
Irregular menstrual bleeding, such as bleeding varying amounts at frequent but unpredictable intervals
-
Bleeding between menstrual periods
-
Excessively heavy menstrual periods
-
Vaginal bleeding after menopause
Diagnosis will usually follow an ultrasound or hysteroscopy. They can be removed surgically while the hysteroscopy is being conducted. A small portion of the polyp may be sent for testing to rule out cancer.
Endometriosis
Endometriosis is caused by tissue which acts like the lining of the womb s spreading itself onto other organs in the same vicinity as your uterus. This can be the outside of the uterus, the ovaries, the bowel or the bladder. 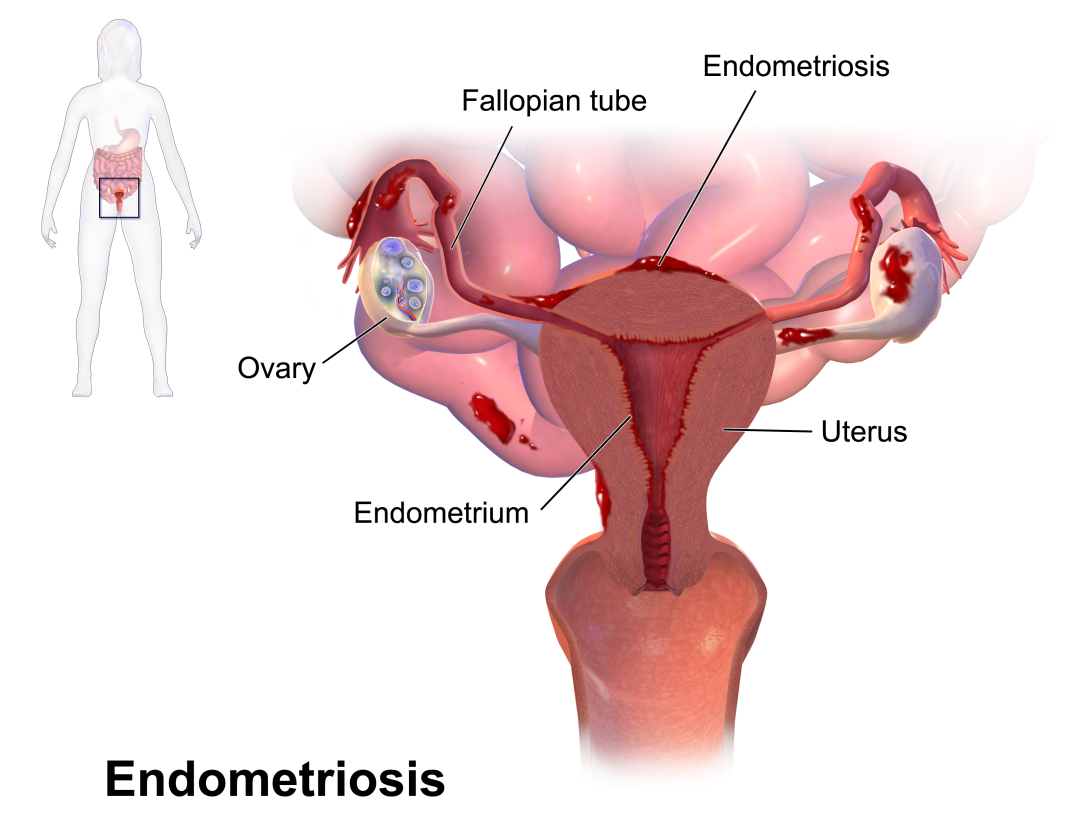
The issue with these cells is they respond in the same way to hormones as your lining does. They grow and shed in response to these hormones. This causes bleeding and a lot of inflammation and pain. Symptoms include:
- period pain that it isn’t helped by a painkiller
- heavy periods
- pelvic pain – this may just occur around the time of your period or you may have it all the time (I mean rocking back and forth pain)
- pain during and after sex
- pain or discomfort when going to the toilet
- bleeding from your bottom or blood in your poo
- feeling tired all the time
Or you could not notice any of these. Which isn’t helpful.
If you think you have endometriosis I cannot stress the need to go to your doctor as soon as possible. If you can (and let’s face it, some of us will need to wait a few weeks) use the NHS symptom diary to take along with you. Take your charts. Take anything you think is relevant. So far the average of 8 years to diagnose this issue is not good enough and if you think you have it you are going to need to be proactive.
Part of the reason it’s so hard to diagnose is that it’s hard to find. The only sure way you can see if a patient has it is to perform a laparoscopy which involves a camera being inserted using keyhole surgery into your womb which isn’t something they’re going to do unless they’re pretty sure you have it and on the assumption that it’s seriously affecting your quality of life. 
Unfortunately endometriosis is not ‘curable’ per say (although there are certain hormonal treatments which are currently on trial which include putting the body into the menopause to kill all cells for 6 months) but there is help available if they find it. This includes:
- anti-inflammatory painkillers like ibuprofen
- hormone medicines and contraceptives including the combined pill and medicines called gonadotrophin-releasing hormone (GnRH) analogues
- laser surgery to cut away patches of endometriosis tissue
- an operation to remove part or all of the organs affected by endometriosis – such as surgery to remove the womb (hysterectomy)
The latter is not so useful for those women who want children. It’s not a great thing to have if you’re trying to conceive but like anything gynaecological, it’s not game over yet. Surgery will often be suggested and many women have found their endometriosis has improved after their first child is born.
For more information please see the NHS website and the Endometriosis UK website.

